ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-I
Clinical effect of open reduction and internal fixation and steinmann pin poking close reduction axial direction, horizontal semi-tublar rivet internal fixation treating sanders II, III calcaneal fracture
Department of orthopedics, The First Affiliated Hospital of Zhejiang University, Zhejiang, 310000, China
- *Corresponding Author:
- Xiangjin Lin
Department of orthopedics
The First Affiliated Hospital of Zhejiang University
Zhejiang, 310000, China
Accepted date: February 01, 2017
Objective: To compare the clinical effects of two kinds of internal fixation methods in the treatment of Sanders II and type III calcaneal fractures.
Methods: 80 patients with Sanders from January 2015 -2016 year in January in our hospital were II-III type of calcaneal fractures, according to number table method, all patients were randomly divided into two groups by treating physicians, the steinmann pin group underwent steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation, Open reduction group underwent conventional open reduction and internal fixation. Observe two groups of patients in hospital stays and costs; X-ray measurement of calcaneus Böhler angle, Gissane angle 2 months treatment before and after; Incidence of complications after 3 months of operation; two groups of patients with Maryland score after the operation of 1 years.
Results: the hospital stay and cost in steinmann pin group was significantly superior to that of the open reduction group (P<0.05); comparing the two groups of patients for 1 year Maryland scores, the pain, line, single item score and total score function in STEADITE needle group was no significant difference from the groups of patients with open reduction (P>0.05); the clinical curative effect of Steinmann pin patients was significantly higher than the open reduction group (P<0.05); the two groups of patients after treatment of Bohler angle and Gissane angle were significantly improved after treatment (P<0.05); the two groups of patients before treatment, Bohler 2 months after the treatment of angle, Gissane angle comparison, no statistically significant difference (P>0.05), compared two groups of postoperative complications, STEADITE needle group after treatment, complication rate (12.5%) was significantly lower than that of the open reduction group (30%), the difference was statistically significant (P<0.05).
Conclusion: In this study, we performed traditional open reduction and steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation for the treatment of Sanders type II-III patients with calcaneal fractures, patients can obtain good clinical curative effect after operation, steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation can be shortened the duration of hospitalization, reduce hospitalization costs and lower incidence of postoperative complications, it is suitable for clinicians to choose the application.
Keywords
Internal fixation methods, Calcaneal fractures, Steinmann pin poking
Introduction
Different types of fractures can be clinically divided as surgical and non-surgical. The characteristics of conventional open reduction surgery is an accurate reduction, a reliable fixation and any complications caused by external fixation can be avoided effectively, Meanwhile, it provides a favourable recovery conditions for the postoperative limb function [1].
Calcaneus fractures are one of the most common fracture that takes place in the tarsal bones is known as Calcaneus fracture. There is still a controversial thought on which would be the best way to treat such disabling injuries. On the other hand, owing to a better knowledge and understanding of the patterns of fracture with the help of the tomography scans that have been computed and the latest surgical techniques have resulted in improvement in the outcome and brought down morbidity and has also paved way for a trend of Open Reduction as well as Internal Fixation. On the other hand, owing to the modern surgical techniques a better understanding of the patterns of fracture along with tomography scans has paved way towards a lowered morbidity and also a trend favouring Open Reduction and Internal Fixation (ORIF) which can be applied to displaced and intra-articular calcaneus fractures. Often the Calcaneus fractures result in different deformities like widening of the heel, losing of the cancaneal height and incongruency of subtalar joint. ORIF can therefore be used for the purpose of addressing these kinds of deformities and also for the purpose of restoring and correcting the anatomic morphology of its calcaneus and so ensuring the biomechanics and the functioning of the hind foot is completely restored [2].
While treating these fractures in the tibial plateau substantial emphasis has to be given in strictly adhering to the anatomical reduction, early movement and rigid fixation principles. At the operation a direct reduction is required for periosteal stripping and in case of stable internal fixation considerable dissection becomes necessary and that, results in the sacrifice of vascular supply. The above techniques has been associated with high degree of complication along with nonunion and also frequently needs secondary bone grafting to be done for bringing down a particular problem [3]. The patient's trauma is large due to open reduction and internal fixation, the fracture of the periosteum and blood transport cause certain damage, and in severe cases can lead to nonunion or delayed healing.
Intra articular Calcaneum fractures was classified by Sanders and is now used widely owing to the manner in which it proved the correlation with management and its prognosis. Treatment of Calcaneum fractures is extremely challenging for an orthopaedic surgeon [4]. The Minimally Invasive Reduction and Osteosynthesis System (MIROS) has proven to be a percutaneous angle stable device which is used for treating fractures. The main objective of this work now is the evaluation of the radiographic and the clinical results of an Osteosysthesis done with the help of MIROS device which is also minimally invasive. 40 consecutive patients totally underwent treatment for intra-articular fracture in the calcaneus. An evaluation of the radiographic and the clinical outcomes post treatment of intra-articular calcaneal fractures making use of the MIROS hardware was made. Damage to soft tissue was observed. On completion of the Orthopaedic Foot and Ankle Society survey for a period of 12 and 24 months a radiologic evaluation was also conducted. There was a significant association in statistical terms between the score of the American Orthopaedic Foot and Ankle Society and a type of soft tissue lesion. Type II, III, and IV fractures of A Sanders was observed in 15, 20, and 15 out of 50 fractures. In a postoperative condition the restoration of posterior facet had reached in 13 of 15, 18 of 20, and 11 of 15 in the case of type II, III, and IV fractures. The American Orthopaedic Foot and Ankle Society scale had a mean score of 85 when the final follow-up visit was made. There was no noticeable connection between the preoperative variables (p>0.09) and the actual score in spite of the bilateral fracture patients having a relatively lower score. This MIROS device for immediate treatment of any intra-articular calcaneus fracture had some very good radiologic and clinical results. The technique that was standardized further reported that with the help of elastic wires that act as girders for the subtalar joint that is displaced due to the fracture and also the lateral calcaneal wall which has collapsed has allowed weight bearing at an early stage, as positive stimuli for the healing of the bone. The percutaneous wires have a drainage effect which is most likely to prevent the compartment syndrome while applying them within the first few hours post the trauma [5].
Bone fractures are common clinical, Sanders II-III calcaneal fractures can lead to the partial displacement of posterior articular surface, because of its unique anatomical structure, the soft tissue of the fracture should be peeled off during the operation, and it is easy to cause the complication such as the stimulation of the nerve, which has a certain effect on the limb after operation [6]. Minimally invasive technique has been widely used in the treatment of fractures, and the corresponding Sanders II-III type of calcaneal fractures treatment options, there is still no uniform standard [7]. In this study, 80 cases of Sanders II- type III calcaneal fractures were treated with traditional open reduction with internal fixation and steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation, to observe and compare the clinical curative effect, report as follows now.
Data and Methods
General information
A total of 80 cases of Sanders II - type III calcaneal fractures treated in our hospital from January 2015 January were selected, Inclusion criteria: all patients were fresh closed fractures; after admission, all the fractures were diagnosed as Sanders type II - III calcaneal fractures by axial position, lateral X ray and CT coronal scan; limb blood flow is normal; exclusion criteria: open calcaneal fractures; sanders of type IV calcaneal fracture; the local soft tissue condition is poor; history of calcaneal fracture or surgical history in the past; ankle fracture; coagulation disorder; mental disorders do not accept surgery.
according to number table method, all patients were randomly divided into two groups by treating physicians, including 40 cases steinmann pin group who underwent steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation, 28 cases were male, 12 were female, aged 19-62 years old, average 41.19 + 9.84, Sanders type II is 29 cases, Sanders type III is 11 cases. 40 cases in open reduction group underwent traditional open reduction and internal fixation, 26 cases were male, 14 were female, aged 18-63 years old, average 43.98 + 8.17, Sanders type, 27 cases of type II and III in 13 cases. The two groups in sex, age, Sanders general data type are compared, the difference was not statistically significant (P>0.05). Two groups of patients and their families have signed the informed consent and the consent form, while the research content and process are approved by the medical ethics committee of scholasticism and supervision.
Method
Preoperative preparation, surgical treatment of the two groups of patients were performed on the side of the axis and the front full back of the X-ray imaging examination, and related indicators were measured. Steinmann pin group were treated with steinmann pin poking closed reduction axial combined with lateral multiple hollow screws internal fixation, this group of patients underwent spinal anesthesia and epidural anesthesia, C arm fluoroscopy with steinmann pins along the longitudinal axis and inclined to drill into the calcaneal, drilling into the point above the Achilles tendon lateral calcaneal tubercle. X-ray observation, the steinmann pin was slowly drilled to stop sinking fracture block below the drill and keep the plantar flexion, the operator uses the other hand to pick out the reset, folding on the broken end of the two fracture, resetting collapsed articular surface and the restoration of the articular surface is smooth. The assistant carries on the extrusion to the patient's bone and recover the width of the normal heel.
Application of Kirschner wire will fracture the fracture line in the vertical straight fixed again. Applying C arm X-ray machine Perspective again, If fracture reduction is satisfactory, then needle on the outside of the Achilles tendon, drill the coarse needle along the longitudinal bone, and wear to the posterior articular surface, run to calcaneal anterior chamber in the middle of calcaneus gradually, The rough guide pin has been used under the lateral to choose another point the same coarse needle vertical drill. From the outside direction of the medial calcaneal direction, calcaneal fractures of the body to wear line in front side of calcaneus. Then apply 2 pieces of appropriate thickness of the transverse guide pin from the outside to the inside through the thalamus or after the articular surface fracture, drill into the value of medial wall before waving calcaneal sustentaculum, posterior articular surface and fine needle in parallel.
The operator view the guide wire position by the C arm X-ray machine perspective, after smoothing the needle position with transverse screw in 2 × 4.5 mm diameter hollow nail, Hollow screw with 2 × 6.5 mm diameter through thick guide pin. Open reduction and internal fixation with traditional open reduction and internal fixation, incision for the lateral extension of the calcaneal "L" shape, under the direct vision to reset the fracture block and the inferior articular surface, fracture of articular surface with bone defect and bone defect were treated with bone graft support. For the postoperative open reduction group, cold compresses is applied to calcaneal area, and treated by conventional antibiotic treatment. In the steinmann pins group, the patients were fixed with high polymer plaster for 1 month. After 1 month’s surgery, patients did limb functional exercises. 2 months after the operation, the patient was able to walk with proper weight.
Observation index
Observe the hospital stay and expenses of two groups of patients. Before and after two months treatment, take a test of calcaneus Böhler angle and Gissane angle by X-ray and observe the complication within 3 months after the operation. Maryland score the two groups of patients within 1 year after the surgery. Maryland rating is the foot scoring criteria made by The American association of Ankle Injuries [8], 100-90 scores for excellent, 89-80 scores for good, 79-70 scores for faire and 69-0 for fail.
Statistical method
By adopting the data statistic software of SPSS19.0, a database is built for statistical analysis. Measurement data is given by (?x ± s), tested by t; enumeration data is given by ratio (%), tested and compared by χ2, IF P is less than 0.05, then there is statistical significance.
Result
Compared with the hospital stay and expenses of the two groups of patients, both the length of the stay and cost of Steinman pin group are obviously less than that of incision reduction group. The difference shows a statistical significance (P<0.05) (Table 1).
| Groups | Case Number | Hospital stay | Hospital Cost |
|---|---|---|---|
| Steinman pin group | 40 | 9.03 ± 1.27 | 1.16 ± 0.23 |
| Incision reduction group | 40 | 12.49 ± 2.04 | 1.69 ± 0.52 |
| t | 4.7951 | 2.3346 | |
| P | <0.05 | <0.05 |
Table 1. The comparison of the hospital stay and expenses of the two groups.
To compare the Maryland scores for the two groups within one year after the surgery, there is no significant difference between the Steinman pin group and incision induction group both in the individual domain scores and total scores for pain, alignment and function (Table 2).
| Groups | Pain | Alignment | Function | Total Scores |
|---|---|---|---|---|
| Steinman pin group | 37.09 ± 5.12 | 8.94 ± 1.92 | 48.21 ± 2.67 | 93.43 ± 8.17 |
| Incision reduction group | 36.98 ± 6.53 | 8.57 ± 2.05 | 48.04 ± 3.73 | 92.91 ± 9.62 |
| T | 0.8749 | 0.7728 | 0.5012 | 0.9703 |
| P | >0.05 | >0.05 | >0.05 | >0.05 |
Table 2. The comparison of the Maryland scores for the two groups within one year after the operation.
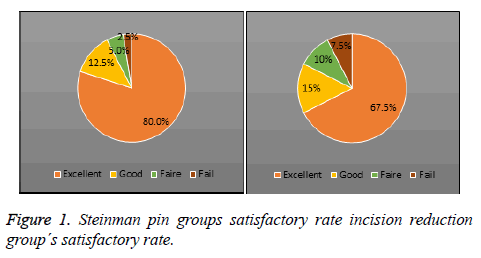
Clinical efficacy evaluation indicates that the satisfactory rate of the clinical efficacy for Steinman pin group is obviously higher than that of incision induction group, which shows statistical significance (Table 3 and Figure 1).
| Groups | Case number | Excellent | Good | Faire | Fail | Satisfactory rate |
|---|---|---|---|---|---|---|
| Steinman pin group | 40 | 32 (80.0%) | 5 (12.5%) | 2 (5.0%) | 1 (2.5%) | 92.50% |
| Incision reduction group | 40 | 27 (67.5%) | 6 (15.0%) | 4 (10.0%) | 3 (7.5%) | 82.50% |
| X2 | 3.2296 | |||||
| P | <0.05 |
Table 3. The comparison of the satisfactory rate of the clinical efficacy for the two groups.
After the surgery, the Bohler angle and Gissane angle for both groups of patients got improved. The difference shows statistical significance (P<0.05); Compare the Bohler angle and Gissane angle before the treatment and 2 months after the treatment for the patients. The difference shows no statistical significance (P>0.05) (Table 4).
| Groups | Böhler Angle | Gissane Angle | ||
|---|---|---|---|---|
| Before Treament | After Treatment | Before Treament | After Treatment | |
| Steinman pin group | 5.23 ± 4.79 | 28.46 ± 5.93 | 161.96 ± 4.82 | 128.11 ± 7.45 |
| Incision reduction group | 5.31 ± 5.17 | 29.14 ± 3.75 | 161.03 ± 5.29 | 128.72 ± 6.32 |
| t | 0.7127 | 0.6385 | 0.8914 | 0.4836 |
| P | >0.05 | >0.05 | >0.05 | >0.05 |
Table 4. The comparision of the Böhler angle and Gissane angle before and after the treatment for the two groups.
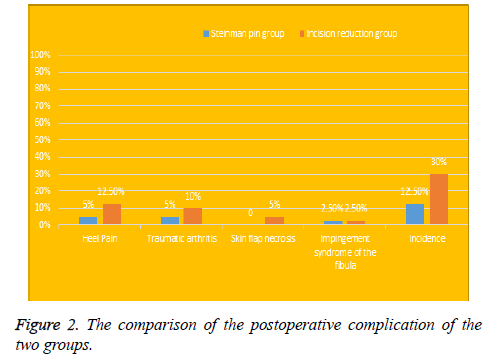
The comparison of the postoperative complication of the two groups shows that the complication rate of the Steinman pin group (12.5%) is obviously lower than that of the Incision induction group (30.0%). The difference shows statistical significance (P<0.05) (Table 5 and Figure 2).
| Groups | Case Number | Heel Pain | Traumatic arthritis | Skin flap necrosis | Impingement syndrome of the fibula | Incidence |
|---|---|---|---|---|---|---|
| Steinman pin group | 40 | 2 (5.0%) | 2 (5.0%) | 0 | 1 (2.5%) | 12.50% |
| Incision reduction group | 40 | 5 (12.5%) | 4 (10.0%) | 2 (5.0%) | 1 (2.5%) | 30.00% |
| X2 | 4.9187 | |||||
| P | <0.05 |
Table 5. The comparison of the postoperative complication of the two groups.
Discussion
At present, the clinical treatments for bone fracture mainly include the fracture reduction, fracture fixation and functional exercise. After the reduction of fracture, fixation should be taken to stop the dislocation and besides, and functional training should be encouraged to prevent complications such as muscle atrophy, synarthrophysis and so on. Calcaneal fracture is a relatively common problem. In the past, incision reduction and internal fixation is usually taken to treat calcaneal fracture patients [9]. However, this method will cause large truama to patients and complications such as skin flap necrosis, incision infection, delay healing or disunion could occur after the operation [10].
Poking reduction can be adopted under C arm X-Ray machine to treat calcaneal fracture. Insert the steel needle into the fracture site, reduce the fracture and then fix the part by the steel needle effectively which could cause less trauma and shorter treating period. After the closed reduction or poking reduction by percutaneous k-wire, then apply cannulated screws to conduct an internal fixation which will get a satisfactory reduction and fixation with the least trauma, conforming to minimally invasive requirements by clinical medicine. According to different Sanders types, different therapeutic methods for calcaneal fracture are conducted [11]. The classification standard of Sanders types are divided by coronal CT and axial imaging condition. And the intra-articular calcaneal fracture is classified on the basis of different fracture situation of caudal articular facet. Calcaneus can be equally divided into three column, and posterior articular facet can also be equally divided into 3 area in terms of the AB lines parallel to the vertical axis of calcaneal bone, which will generate three potential fracture blocks: laterals ide, central side and inner side. This classification standard can effectively reflect the damage situation of posterior calcaneal facet of different patients. To divide the fracture situations of patients rationally could help implement diagnostic treatment for patients according to different classification and improve the prognosis effect largely [12,13]. In this study, calcaneal fracture is classified into Sanders II, Sanders III fracture and obvious fracture displacement.
Previously, conservative management is mainly applied to treat calcaneal fracture clinically. However, with the development of medical science, incision reduction and internal fixation and poking reduction and internal fixation are mainly conducted to treat Sanders II and Sanders III fracture clinically. Incision reduction and internal fixation can not only realize anatomical replacement at the maximum extent, helping recover the calcaneal bone to normal shape, but also prevent the traumatic arthritis and other complications [14]. Lateral extension of “L” incision is mainly adopted in the method of incision reduction and internal fixation, which can cause less truama around the fracture structure, decreasing the damage for the surrounding blood vessels, nerve and muscle tendon in the direct reduction fracture block and subtalar joints. Reduce repeated reset operation in the treatment as far as possible, pay close attention to shorten operation time, and bring down the occurrence of compartment syndrome to enhance the postoperative recovery [15].
Poking reduction and internal fixation is actually a closed reduction under perspective cases, which can cause less damage on patients [16]. In this study, there is no obvious difference in the pain and function between the two groups of patients. Bohler angle and Gissane angle of both two groups of patients get obvious improvement and there is no distinct difference in the recovery of the two angles before and after the treatment. Tip: For Sanders II and Sanders III fracture patients, both the traditional method of incision reduction and internal fixation and Steinman pin poking closed reduction and cannulated screws internal fixation can obtain satisfactory clinical results, which implement positive effect on the foot recovery. The result of this study shows that the hospital stay and expenses of the Steinman pin group is obviously shorter and lower than that of incision reduction, and the complications are also less, which could be explained that less trauma around the fracture structure in the Steinman pin reduction and closed fixation is beneficial to the postoperative recovery. The result also indicates that there are two cases of skin flap necrosis in the incision reduction group while no such cases occur in the Steinman pin group which can be explained that there is no large damage to local soft tissues during the Steinman pin reduction and relatively less complications. However, this study suggests that there are some shortcomings in the Steinman pin reduction including the requirement for repeated X-Ray perspective reduction, blur sight of the broken end and inconvenient displacement and reduction for posterior articular facet. As for the deficiency of cases and observation indexes, there might be a negative impact on the result and conclusion of this study. As a result, it is necessary to enlarge the sample size and increase observation time.
In conclusion, in this study, traditional incision reduction and Steinman pin poking reduction and internal fixation are separately conducted on patients of Sanders II and Sanders III calcaneal fracture. Both groups of patients get satisfactory clinical effect. However the method of Steinman pin poking reduction and cannulated screws internal fixation is a better choice for clinicians since it could help shorten the hospital stay, reduce the hospitalization expenses and complications.
References
- Zhao Z, Shang XF, Zhou XS. Clinical Analysis on Different Treatment Methods of Calcaneal Fracture. Chinese J General Practice 2013; 11: 18-20.
- Mostafa MF, El-Adl G, Hassanin EY, Abdellatif MS. Surgical treatment of displaced intra-articular calcaneal fracture using a single small lateral approach. Strategies Trauma Limb Reconstruct 2010; 5: 87-95.
- Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg Br 2009; 91: 426-433.
- Nimmagadda KP, Kolla S, Vithala S. Study of Functional Outcome in Calcaneal Fractures. IOSR J Dental Med Sci 2014; 1: 100-107.
- Battaglia A, Catania P, Gumina S, Carbone S. Early minimally invasive percutaneous fixation of displaced intra-articular calcaneal fractures with a percutaneous angle stable device. J Foot Ankle Surgery 2015; 54: 51-56.
- Li JL, Qian Y, Liang WQ. Comparidon of effect between closed reduction hollow screw fixation and anatomic calcaneal titanic plate fixation for treatment of Sanders type ? calcaneal fracture. Chinese J Bone Joint Injury 2014; 29: 1242-1244.
- Xu HD, Zhao JN, Chen Y. Comparison of curative effects of two kinds internal fixation in treating calcaneal fractures. Chinese J Bone Joint Injury 2013; 28: 128-130.
- Li JG, Chen XJ, Lv WB. Percutaneous poking reduction versus open reduction for internal fixation of Sanders ?/? calcaneal fractures. Orthopedic J China 2016; 24: 1449-1455.
- Wallin KJ, Cozzetto D, Russell L. Evidence-based rationalefor percutaneous fixation technique of displaced intra-articularcalcaneal fractures: a systematic review of clinical outcomes. J Foot Ankle Surg 2014; 53: 740-743.
- Hao X, Wei L, Wei-Wen L. Comparison of therapeutic effects of implant internal fixation for the treatment of Sanders? calcaneal fractures after poking and open reduction. Chinese J Tissue Eng Res 2013; 17: 4919-4925.
- Qu F, Yuan B, Qi W, Wang J, Shen X, Wang J, Zhao G, Liu Y. Poking reduction treatment of displaced scapular neck fracture with shoulder arthroscopy-assisted surgery. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014; 28: 798-801.
- Li Y, Liang X, Wang L. Short-term efficacy of treatment on part intra-articular calcaneal fractures by open reduction andcannulated screw internal fixation with small incision and bone grafting. Chinese J Bone Joint Surgery 2012; 5: 401-404.
- Kinner B, Kerschbaum M, Bley C, Spiegel A, Roll C. Bionic plate design for calcanealfracture treatment : a biomechanical analysis and first clinical results, Int Orthop 2015; 39: 111-117.
- Zeng XT, Shu HS, Wang HC. Treatment of intraarticular calcaneal fractures using poking reduction combined with Ilizarov method. Chinese J Trauma 2011; 27: 537-540.
- Tang SY, Zhu XM, Yang H. Analysis of correlation between reduction quality of posterior subtalar articular surface and curative effect of calcaneal fracture. Orthopedic J China 2015; 8: 1448-1453.
- Bussewitz BW, Hyer CF. Screw placement relative to the calcanealfracture constant fragment: an anatomic study. J Foot Ankle Surg 2015; 54: 392-394.