ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2013) Volume 24, Issue 3
Awareness, utilization and attitudes towards emergency contraception among women attending at a primary health care clinic in Durban, South Africa.
1Department of Health Studies, University of South Africa
2Graduate School of Business and Leadership, University of KwaZulu-Natal (Westville Campus) South Africa
- Corresponding Author:
- M. E. Hoque
Graduate School of Business and Leadership
University of KwaZulu-Natal (Westville Campus), South Africa
Accepted Date: March 14 2013
Citation: Naidoo U, Zungu L, Hoque ME. Awareness, utilization and attitudes towards emergency contraception among women attending at a primary health care clinic in Durban, South Africa. Biomed Res- India 2013; 24: (3): 341-346.
A high level of unwanted pregnancies among young women is an urgent public health problem in South Africa. The study sought to establish awareness, utilisation, and attitude towards the use of emergency contraception (EC) among patients seen at the Commercial City Reproductive Health Clinic in Durban, South Africa. A cross-sectional descriptive study was conducted by means of a self-administered questionnaire among 103 sexually active females between the ages of 18-49 years. More than two-thirds (72.8%) of the participants heard about EC and among them 85.3% had used EC. Among those who heard about EC, 53.3% of them heard about are from clinics. About two-thirds (63.1%) participants knew the correct timing when EC should be taken following sexual intercourse, and majority (73.7%) indicated that EC is used to prevent unplanned pregnancy. Majority (77.6%) of the participants displayed a positive attitude towards the use of EC. About a third (31.1%) of the participants reported that EC was against their cultural beliefs or religions. Majority (82.5%) also indicated to recommend EC to other women as a family planning method. Awareness of utilisation of EC was good among the participants. Most of the women displayed positive attitudes towards EC and perceived it to be beneficial. Health professionals should inform and alert women/clients on the consequences of unprotected sex, and guide them to make informed choices by means of adequate information regarding EC.
Keywords
Awareness, utilisation, emergency contraception, South Africa
Introduction
Emergency contraception (EC) refers to methods that women can use to prevent pregnancy after unprotected sexual intercourse, and is also known as “post-coital” contraception [1]. Situations of unprotected intercourse where EC can be used as a backup contraceptive method include, failure of barrier methods such as slippage, breakage or misuse of the condom, sexual assaults, rape, failed coitus interruptus, two or more consecutive missed oral contraceptive pills, or simply because intercourse was unexpected and therefore contraception had not been used [2]. Worldwide unplanned pregnancy is a major medical, social, and public health problem [3]. There are 80 million unplanned pregnancies in the world every year, of which 38% of all pregnancies can be deemed an epidemic [4]. The WHO estimates that about 46 million abortions are performed under unsafe conditions [5]. There is growing worldwide acceptance and promotion of EC as a measure to reduce the level of unwanted pregnancies and, hence, unsafe abortion.
In an American study, it was reported that nearly half of all pregnancies were unintended and half of these pregnancies end in elective termination [6]. Another study highlighted the potential effect of EC in this regard could be most evident in sub-Saharan Africa [7]. Women in low income and minority groups are at highest risk of unintended pregnancy have limited access to primary care and may have difficulty accessing highly effective contraception [8]. It was reported from a Nigerian study that EC could play an important role in averting pregnancies attributable to non-use or incorrect use of contraceptives, contraceptive failure, lack of knowledge about, or access to methods, or coerced sex [2].
High pregnancy rates are common among adolescent populations in South Africa, emphasising the need for sexual health education and family planning education. It was reported that 78% of births to women 19 years of age and younger were unplanned [1]. Another multisituational analysis from three provinces revealed that the large proportion of women (65%) had a pregnancy when they were not ready [9]. Ibisomi and Odimegwu showed that only 29% pregnancies among 15-29 years old women in South Africa were wanted [10]. Other South African researchers have stated that although several contraceptive methods, including EC are freely available to users at all public sector health facilities across the country, high rates of teenage and unintended pregnancies persist in South Africa [11]. EC is the only form of contraception that can reduce the risk of pregnancy after unprotected intercourse or when a planned contraceptive method fails.
EC is highly effective in preventing an unintended pregnancy if taken within the recommended time limits. The high rate of teenage and unintended pregnancies at Commercial City Reproductive Health Clinic (CCRHC) is an area of concern especially in the light of the HIV/AIDS epidemic in KwaZulu-Natal province of South Africa. This clinic specialises in reproductive health care. The aim of this study was, therefore to assess awareness, utilisation, and barriers of women attending a local reproductive clinic in Durban Metropolitan area regarding the use of EC.
Material and Methods
Design and setting
This was a descriptive, cross-sectional study conducted at a CCHRC in Durban. The clinic is a specialised youth and adult clinic that offers a limited range of services including family planning/child spacing. The clinic is ideally situated in the Central Business District (CBD) and services most of the working population, street vendors, scholars and visitors to the CBD. Clients attending the facility have easy access and other services not offered at the clinic are within a 10km radius following referral for appropriate care. The clinic offers services to an average of 4500 clients per month. The following services are offered at this site: sexually transmitted Infections (STIs) management and treatment, rape crisis, counselling and termination of pregnancy (TOP) referral, Health education, family planning and contraception, diagnostic screening e.g. pap smears, and HIV counselling and testing. This clinic was chosen due to the nature of contraceptive services offered in terms of sexual and reproductive health (RH) and the underutilisation of EC among service users.
Population, sampling and sample size
The target subjects for the study were all the female patients who attended the clinic for the purpose of family planning and contraception. The study population included women only and the inclusion criterion was sexually active females between the ages of 18-49 years old.
The average number of clients attending the health facility for family planning and contraception per month (20 days) is 1625. From this target population, the sample size of 91 was obtained based on the followings: 50% of the population used EC (since prevalence of EC used was unknown), worst acceptable at 40% giving the statistical power of the study as 80%. Another 15% was added to the sample because of non-response. So the final sample size for the study was 104. Simple random sampling was used to select the samples. Everyday six (6) clients were randomly selected using random numbers for the first three weeks from 23 August 2010 and the last week ending to 17September 2010, each day three clients were selected. The subjects were selected by the researcher over a period of 4 weeks (20 days), from Monday to Friday.
Ethical considerations
Ethical approval for the study was obtained from Research and Ethics Committee of Department of Health Studies, University of South Africa. Permission was requested and obtained from the Department of Health, South Africa and from the clinic manager to conduct the study at the CCHRC. Informed consent form was signed and obtained from all the participants. Participation in this study was voluntary and the subjects were allowed to withdraw from the study without any penalty imposed on them. The participants’ right to confidentiality was protected; all questionnaires were identified only by a number and no identifying information was appended to research materials, therefore no information could be traced back to them. All confidential information was kept at a place where nobody had access to it except the researcher.
Data collection
A self-administered questionnaire was used to collect data. The researcher identified the selected participants and the research assistant who was trained in the selection process, invited the women to participate in the study. The purpose of the study was explained to the respondents. The respondents were directed to a quiet place within the clinic and were asked to complete the questionnaire individually to avoid influence from one another. Those who were illiterate, the research assistant asked the question and completed the questionnaire. Participants were asked to place the completed questionnaire in a labelled box provided at the auxiliary officer’s desk. The questionnaires were collected at the end of each day by the researcher and locked in a filing cupboard. The research assistant ensured the clients did not lose their place in the queue by observing the numbering system closely.
A pilot study was conducted on five women who were not part of the main study. This provided insight into the interpretation and understanding of the questions asked. The pilot study was also conducted to determine the feasibility and clarity of the questions posed, consistency in the data collection procedure thereby ensuring validity and reliability in the data collection tool.
Data analysis
Data were entered into a Microsoft Excel 2003 spread sheet and imported to SPSS 18.0 for window version for analysis. All the variables were summarized using descriptive summary measures: expressed as mean (± standard deviation) for continuous variables, and percent for categorical variables.
Results
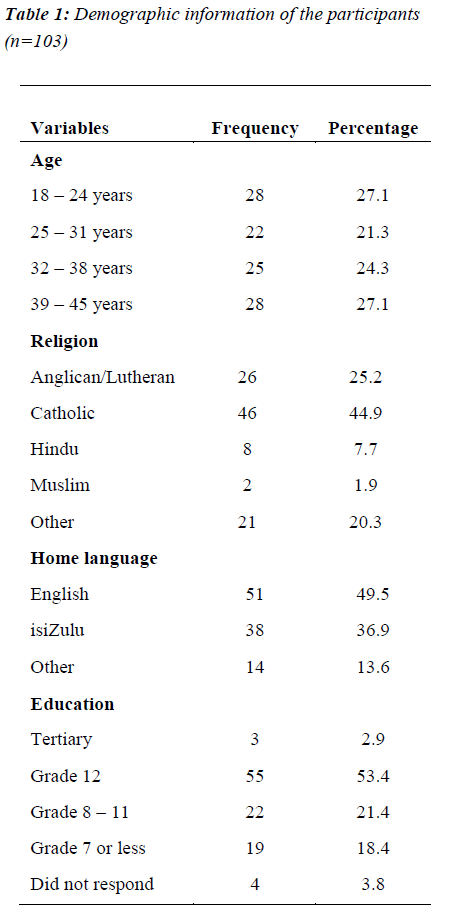
A total of 103 clients completed the questionnaire. Table 1 summarises the socio-demographic information’s of the participants. All (100%) the participants were female, 51.4% were more than 31 years old, 41.7% were catholic, and half of their (49.5%) home language was English. Three clients did not indicate their educational information. More than half (58.6%) indicated that they had attained grade 12 (Matric) or more (tertiary) as their highest level of education.
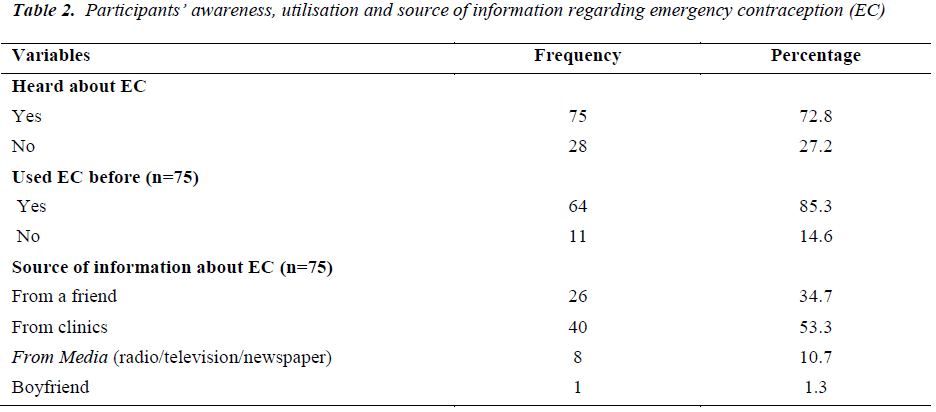
Regarding awareness of EC, about two-thirds (72.8%) of the participants heard about EC. Of those who heard about EC, majority (85.3%) indicated that they had used EC before (Table 2). Participants were asked to indicate the source for acquiring EC information and it was a multiple choice answers provided, where the participants could answer more than one answers. Among those who heard about EC, slightly more than half (53.3%) reported that they heard about EC from clinics. Respondents who were aware of EC most commonly reported that they had first heard about EC from friends or family members (40%), or at clinic (27%)
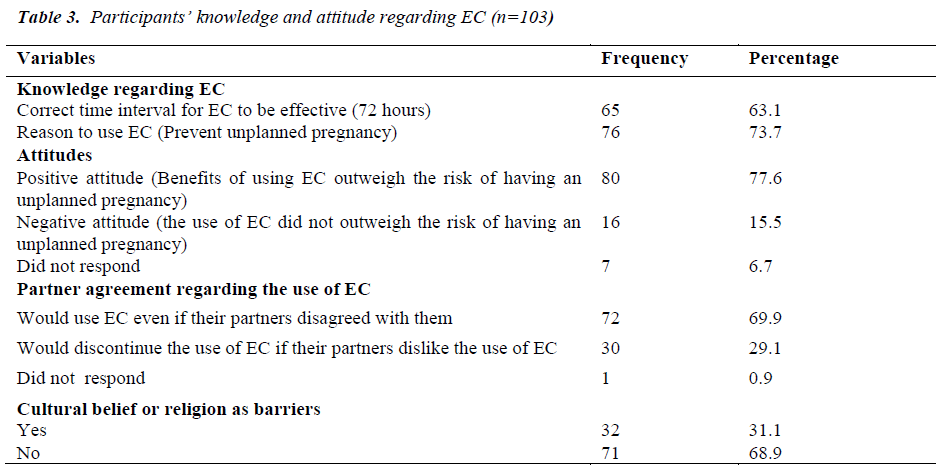
Table 3 reports participants’ knowledge and attitudes towards EC. About two-thirds (63.1%) participants knew the correct time interval that EC should be taken following sexual intercourse, and majority (73.7%) indicated that EC is used to prevent unplanned pregnancy which is correct. Majority (77.6%) of the participants displayed a positive attitude towards the use of EC as they felt that the benefits of using EC outweigh the risk of having an unplanned pregnancy. Participants were also asked to indicate whether they would continue to use EC even if their partners did not agree to this method of family planning and 69.9% indicated that they would use EC even if their partners disagreed with them. About a third (31.1%) of the participants reported that EC was against their cultural beliefs or religions.
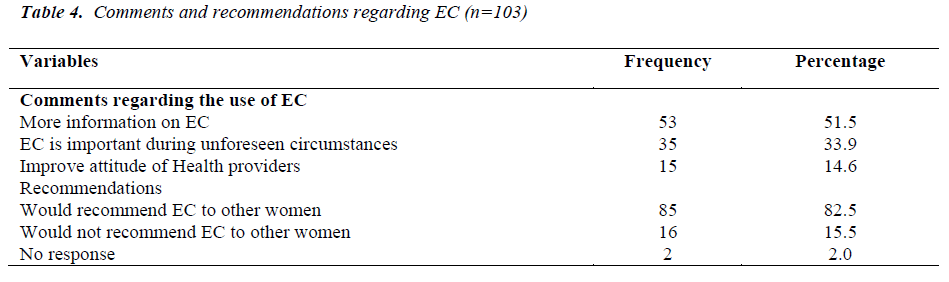
Table 4 shows participants’ comments and recommendations regarding EC. More than a half (51.5%) of the participants indicated that they wanted to know more about EC, and another 33.9% viewed EC as an important family planning method when certain circumstances prevail, such as rape and unprotected sex. Participants were asked if they would recommend EC to other women as a family planning method and majority (82.5%) of them answered positively.
Discussion
This study investigated awareness, utilisation, and barriers of women attending a local reproductive clinic in Durban Metropolitan area regarding the use of emergency contraception. Majority of the participants were aware of EC, utilized EC and had positive attitudes towards EC. The present study found that majority of the participants heard about EC and had used EC before. This result is higher than previous South African studies. A study in the Western Cape Province of South Africa, reported that the level of EC awareness was particularly low in the rural region with only 17% of women being aware of EC compared with 35% of women in the urban region [9]. Another South African study found that only 17% of the women aged 15-24 years attending public sector health facilities had ever heard of EC [12]. South African study conducted among sexually active women attending public health clinics also reported that 13% ever used EC [11]. The overall awareness is therefore found to be lower in South Africa than data obtained from Europe and North America, but is similar to or higher that what has been reported in other developing countries including Mexico, India, Kenya and Nigeria [11].
Regarding source of information, slightly more than half reported that they heard about EC from clinics. A South African study conducted among pharmacists and doctors regarding EC, highlighted that participants were reasonably informed of the methods, and there is a need to improve their knowledge [13]. This finding is in line with other South African studies which conducted among tertiary students in Durban and women from Western-Cape province [11, 14].
EC is the only form of contraception that can reduce the risk of pregnancy after unprotected intercourse or when a planned contraceptive method fails. Majority of the participants had fairly good knowledge of EC since they knew that EC is used for preventing unplanned pregnancy and also knew the correct time interval that the EC should be taken following sexual intercourse. Since most of the participants heard about EC from clinics, they possibly received proper information from the health care workers. This finding is contrary to other studies conducted in South Africa. Previous South African studies reported low level of knowledge among the participants [11, 14]. In a meta-analysis of EC knowledge, attitudes, and use, researchers reported that while only about 10% of the respondents could spontaneously define the method, al most all females claimed to know what EC was when provided with a brief description or asked to pick it from a list [15].
Majority of the participants in this study displayed a positive attitude towards the use of EC as they felt that the benefits of using EC outweigh the risk of having an unplanned pregnancy. A Cameroonian study reported positive attitude indicating a strong tendency of use of EC in the future by respondents [16]. This is in line with public sector primary health care clients in South Africa and Ghanaian students, who also had similar attitudes [9, 17]. This indicates that the participants are interested in learning more about EC.
Limitations of the study
The study was limited to contraceptive users only and didn’t target women accessing the clinic for STIs or any other gynaecological condition. Therefore, the results of this study cannot be generalised to other settings.
Conclusion
The study revealed that women are aware of the existence of EC and utilised it. Significant number of women had heard of it at the clinic. The findings also indicate that women displayed positive attitudes towards EC and perceived it to be beneficial. Health professionals should inform and alert women/clients on the consequences of unprotected sex, and guide them to make informed choices by means of adequate information regarding EC. In this way they may develop enough trust and self confidence to enable them to take wise decisions with regard to their sexual health.
Acknowledgements
The authors wish to thank the clinic management team for their support to conduct this study; and the patients who voluntarily took part in this study. No funding was received for the study.
References
- Steyn PS, Mason D. Emergency contraception: a review. O & G Forum 2009; 19: 127-133.
- Olufunke ME, Osaretin E, Victor I. Health care providers’ knowledge of, attitudes toward and provision of emergency contraception in Lagos, Nigeria. Intl Fam Plann Perspect 2006; 32: 89-93.
- Kang HS, Moneyham L. Use of emergency contraceptive pills and condoms by college students: a survey. Int J Nurs Stud 2008; 45: 775-783.
- Glasier A, Gülmezoglu MA, Schmid GP, et al. Sexual and reproductive health: a matter of life and death. The Lancet Sexual and Reproductive Health Series, October 2006. Available at: http:// www.who.int/reproductivehealth/publications/general/l ancet_1.pdf
- WHO, Division of Reproductive Health. Unsafe abortion. Global and regional estimates of incidence of and mortality due to unsafe abortion, with a listing of available country data (WHO/RHT/MSM/97.16) Geneva, Switzerland. World Health Organization (WHO), 1998.
- Wallace JL, Weinstein J, Wu J, et al. Emergency contraception: knowledge and attitudes of family medicine providers. Fam Med 2004; 36: 417-422.
- Baiden F, Awini E, Clerk C. Perceptions of university students in Ghana about emergency contraception. Contraception 2002; 66: 23-26.
- Schwarz EB, Gerbert B, Gonzales R. Need for emergency contraception in urgent care settings. Contraception 2007; 75: 285-288.
- Smit J, McFayden L, Beksinska ME, et al. Emergency contraception in South Africa. Knowledge, attitudes, and use among public sector primary health care clients. Contraception 2001; 64: 333-337.
- Ibisomi LDG, Odimegwu CO. Predictors of unintended pregnancy among South African youth. Eastern Africa Social Science Research Review 2007; 23: 61-80.
- Myer L, Mlobeli R, Cooper D, et al. Knowledge and use of emergency contraception among woman in the Western Cape province of South Africa: a crosssectional study. BMC Women’s Health 2007; 7: 14.
- Mqhayi MM, Smit JA, McFadyen ML, et al. Missed opportunities: emergency contraception usage by young South African women. Afr J Reprod Health 2004; 8: 137-144.
- Hariparshad N. Knowledge of emergency contraception among pharmacists and doctors in Durban, South Africa. Eur J Contracept Reprod Health Care 2001; 6: 21- 26.
- Roberts C, Moodley J, Esterhuizen T. Emergency contraception: knowledge and practices of tertiary students in Durban, South Africa. J Obstet Gynaecol 2004; 24: 441-445.
- Ellertson C, Schochet T, Blanchard K, et al. Emergency contraception: a review of the programmatic and social science literature. Contraception 2000; 61: 145-186.
- Kongnyuy EJ, Ngassa P, Fomulu N, et al. A survey of knowledge, attitudes and practice of emergency contraception among university students in Cameroon. BMC Emerg Med 2007; 7: 7.
- Addo VN, Tagoe-Darko ED. Knowledge, practices, and attitudes regarding emergency contraception among students at a university in Ghana. Int J Gynecol Obstet 2009; 105: 206-209.