ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2013) Volume 24, Issue 4
Anatomical variations in the branching of human aortic arch.
1Mevlana University Department of Physical Therapy and Rehabilitation
2Mevlana University Faculty of Medicine Department of Anatomy
3Mevlana University Faculty of Medicine Department of Radiology, 42003 Konya Turkey
- *Corresponding Author:
- Musa ACAR
Mevlana University
Department of Physical Therapy and Rehabilitation
42003 Konya TURKEY
Accepted August 24 2013
Citation: Acar M, Ulusoy M, Zararsiz I, Efe D. Anatomical variations in the branching of human aortic arch. Biomed Res- India 24 (4): 2013; 531-535.
Aortic arch (AA) is a prolongation of aorta ascendens and forms a part of mediastenum superius. It begins right above the joint of sternum and the second rib at the posterior right half of manubrium sterni. Presently, aorta has been pointed out not only to perform the duty of a canal but in fact has been shown to have a significant role in regulating left ventricular function and myocardial perfusion. To be well aware of the arterial patterns of this area is of significant importance in situations that require urgent interventions and cardio-thoracic surgery. The objective of this study was to determine the various different AA branching patterns belonging to Turkish population. We are convinced that the results obtained will be of significant importance to anatomists, chest surgeons and radiologists attempting cardio-vascular intervention. This study was done on 94 patients (32 females 64 males) who had applied to the Radio-diagnostic Department for computerised tomography (CT) angiography, during 2010-2011 at Mevlana University Medical Hospital. In our study, seven different branching patterns belonging to AA were observed. AA was found to give out minimum of two and maximum of five branches. Being aware of this variations and its determination prior to medical intervention would be of vital importance in relation to treatment process of the patient. Therefore we believe that the results obtained in our study will be of particular importance to anatomists, cardio-vascular surgeons, chest surgeons and radiologists carrying out vascular intervention applications.
Keywords
Arcus aortae; multidetector computerized tomography; variation; anatomy.
Introduction
Aortic arch (AA) is a prolongation of aorta ascendens and forms a part of mediastenum superius. It begins right above the joint of sternum and the second rib at the posterior right half of manubrium sterni. It then extends behind, forming a curve towards the left and continues on the lower level of fourth thoracic vertebra as pars thoracica aortae. During the continuation as AA, first one shows convexity upwards, the other one forms two curves projecting towards left anterior. Arteries, nourishing the head, neck and upper thoracic regions originate from this area [1]. AA gives out branches from proximal to distal end into brachiocephalic trunc (BT), left common carotid artery (LCCA) and left subclavian artery (LSA) branches respectively. This branching fashion, known as the classic pattern is seen more frequently as compared to other branching patterns. Besides, ligamentum arteriosum binds AA to left pulmoner artery [2,3,4].
Presently, aorta has been pointed out not only to perform the duty of a canal but in fact has been shown to have a significant role in regulating left ventricular function and myocardial perfusion [5]. Descending aort aneurysms is one of the most important vascular diseases requiring complex surgical intervention. On the other hand, radiologists and surgeons attempting vascular entry in order to reach supra-aortic branches through catheter, also needs to go through AA. In this respect, AA and supraaortic branches hold a great deal of significance for surgeons and other operators. [6].
To be well aware of the arterial patterns of this area is of significant value in situations requiring urgent interventions and cardio-thoracic surgical procedures [1]. The objective of this study was to determine the various different AA branching patterns belonging to Turkish population. We are convinced that the results obtained will be of significant importance to anatomists, cardiovascular surgeons, chest surgeons and radiologists attempting vascular intervention.
Materials and Methods
This study was done on 94 patients (32 females 64 males) who had applied to the Radio-diagnostic Department for computerised tomography (CT) angiography, during the year 2010-2011 at Mevlana University, Medical Hospital. The images were taken from patients who had no problems related to AA, by multidetector computerised tomography (MDCT) angiography method. Patients whose ages ranged from 31 to 86 were included in the study.
In the first part of the study, images of 64 cross-section of MDCT (Siemens Somatom Sensation, Erlanger, Germany, 2005) and AA branching obtained from patients who had applied to the hospital previously were determined. Afterwards, suitable images from sagittal, coronal and axial plane were determined and assessed morphologically in order to evaluate arterial structures from an anatomical perspective. Branching patterns belonging to all specimens and anatomical variations were recorded and frequency of occurence were determined.
Results
In our study, seven different branching patterns belonging to AA were observed. AA was found to give out minimum of two and maximum of five branches. The form of the branches were classified into Type A, Type B, Type C, Type D, Type E, Type F and Type G. The types were numbered serially based on their frequency of occurence, from the most frequent to the least frequent. AA branches were marked in sequence from right to left. Accordingly, AA branching patterns and branches alloted serially were determined in the fashion below.
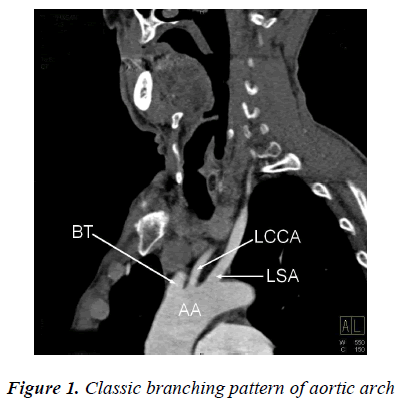
Type A: BT, LCCA, LSA (74,46%) (Figure 1.)
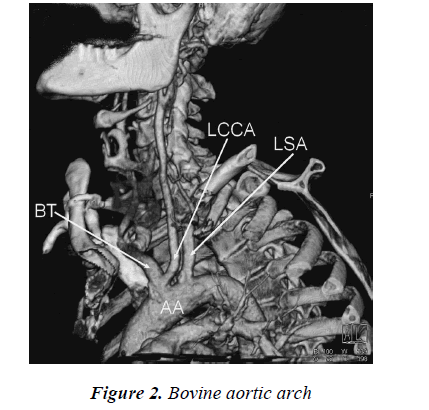
Type B: BT and LCCA common root, LSA (14,91%) (Figure 2.)
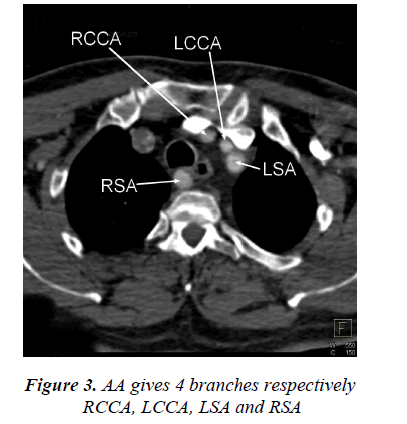
Type C: right common carotid artery (RCCA), LCCA, LSA, right subclavian artery (RSA) (4,25%) (Figure 3.)
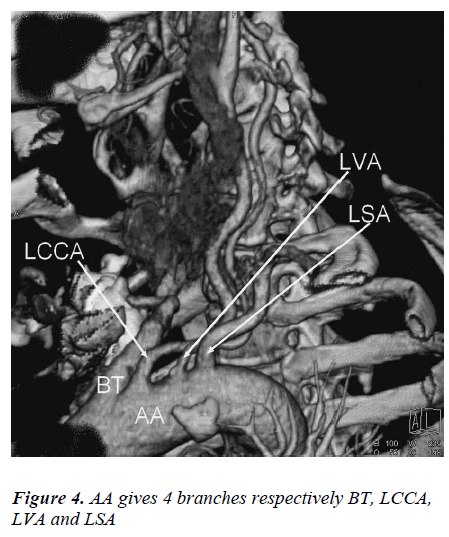
Type D: BT, LCCA, left vertebral artery (LVA), LSA (2,13%) (Figure 4.)
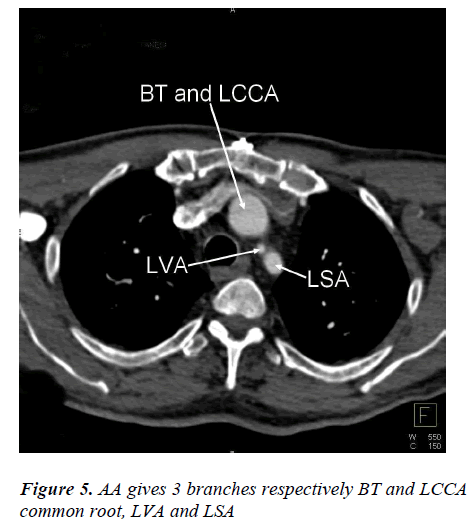
Type E: BT and LCCA common root, LVA, LSA (2,13%) (Figure 5.)
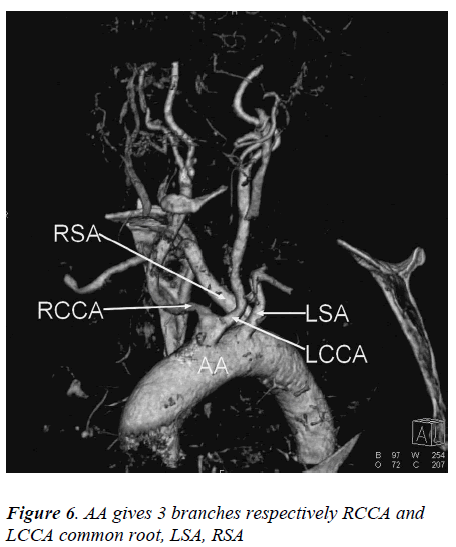
Type F: RCCA and LCCA common root, LSA, RSA (1,06%) (Figure 6.)
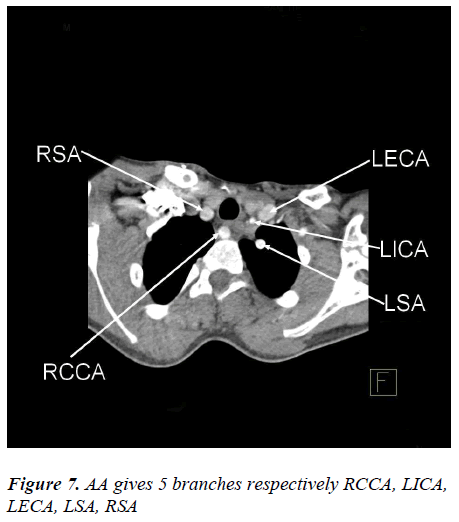
Type G: RCCA, left internal carotid artery (LICA), left external carotid artery (LECA), LSA, RSA (1,06%) (Figure 7.)
Discussion
Abnormal branching patterns of AA may adversely affect hemodynamic balance leading to cerebral abnormalities [3]. Anatomic variations of this area is of significant importance for vascular radiology interventions and applications of surgical procedures [7]. The most frequent branching pattern seen in AA is known as the classic branching pattern giving out branches in BT, LCCA ve LSA branching patterns [8]. In a study performed by Ogengo’o et al, on 113 cadavers, 67,3% were found to be in accordance with classic pattern of AA branching. Natsis et al, have reported the percentage of branching style with intervals to be between 64.9–94.3% of all cases, in the literature. In the same study, 527 cases were radiologically analysed and this percentage was reported to be around 83%. In our study, classic branching pattern termed as Type A was determined in approximately 70 cases (74,46%). This percentage is within the range specified in the literature.
In the studies performed, 30% AA branching cases have been reported to have variational developments. Among these, the most frequently observed variations are BT and LCCA common root variations [10]. This type of branching may also be termed as ‘bovine aortic arch’ [11]. Natsis et al, in their study, have located 15% of bovine aortic arch structures. Szpinda et al, have reported 21% of such structures in their study. In our study, branching pattern termed as Type B was determined to be around 14,91%. This proportion is in parallel to the results recorded by Natsis et al.
In our study, AA pattern termed Type C, which branches off from right to left in the sequence RCCA, LCCA, LSA and RSA branches determined as 4,25% is the third most frequently observed variation. RSA branching into the left of AA has been termed as aberrant subclavian artery or arteria subclavia dextra lusoria (ASDL). This type of branching style is very rarely encountered in the literature. In 80% of cases, ASDL branches pass between columna vertebralis and oesophagus, in 15%, between oesophagus and trachea and in 5% the branches are seen to pass through anterior part trachea [13]. Generally ASDL is asymptomatic, it has been further stated that in cases where arteries may create pressure on oesophagus and trachea, this may lead to situations causing dysphagia or respiratory problems [14].
Vertebral artery (VA) is classically as a branch of subclavian artery (SA). As, in which variations are found. It may separate out from any branch of AA, common carotid artery (CCA), external carotid artery (ECA), internal carotid artery (ICA) or SA [15]. The most frequently reported variational form of VA is, originating of LVA from AA in between LCCA and LSA [16]. In our study, branching pattern which was termed Type D (2,13%), BT, LCCA, LVA and LSA was seen to abandon AA, in sequence. Jakanani et al, in their study reported that 6% of LVA abondoned AA. Haifa et al (17), reported this rate to be 5,5%. This type of branching was encountered in a much lower proportion in our study, as compared to other literature.
VA variations are generally asymptomatic. As a result, it cannot be noticed beforehand. However, anomalies in AA branching pattern may change hemodynamic balance in a way, so as to affect cerebral anomalies. These patterns must be definitely reviewed prior to surgery because unexpected problems regarding circulation may be encountered. For example, in a case where VA is found to separate from CCA, binding of CCA may lead to complications involving bleeding in the brain. As a result, it should be kept in mind that applications involving VA of head and neck areas may cause stenosis and blockages and therefore, it is important to know the point of origin of VA [16,3].
In our study, the branching style that was termed Type E is a combination of Type B and Type D. In this style, which was seen in 2,13% cases, BT and LCCA left AA as a common root and was located just before LVA and LSA. Best et al (18), reported one case where right VA was found to leave from AA. Sunitha et al, recorded the frequency of this case to be 2.6% in their study.
The other branching style observed for ASDL in our study was termed Type F (1,06%). Emerging as the first branch of AA and sharing a common root with CCA (bicarotid trunc) this root follows LSA and RSA in sequence. Natsis et al, determined 0,16% of this style of branching in their study and suggested that bicarotid trunk could result in tracheobronchial compression. Nayak et al (19), encountered this kind of branching style in 1,6 % of cases.
The last type of branching style observed for ASDL was termed Type G (1,06%). In this branching style, AA gave out RCCA, LICA, LECA, LSA and RSA branches respectively. This style was observed only in one single case in our study, however, we did not come across this branching style in literature review performed.
As a conclusion, it was determined that variations belonging to AA is observed quite frequently in the population. Being aware of this variations and its determination prior to medical intervention would be of vital importance in relation to treatment process of the patient. Therefore we believe that the results obtained in our study will be of particular importance to cardiovascular surgeons, chest surgeons and radiologists carrying out vascular intervention applications.
References
- Bhatia K, Ghabriel MN, Henneberg M. Anatomical variations in the branches of the human aortic arch: a recent study of a South Australian population. Folia Morphol 2005; 64(3): 217-23.
- Sunitha V. A Study of aortıc arch ın human fetuses of north coastal andhra pradesh. International Journal of Basic and Applied Medical Sciences 2012; 2 (1):196-200.
- Shiva Kumar GL, Pamidi N, Somayaji SN, Nayak S, Vollala VR. Anomalous branching pattern of the aortic arch and its clinical applications Singapore Med J. 201; 51(11): 182-3.
- Natsis KI, Tsitouridis IA, Didagelos MV, Fillipidis AA, Vlasis KG, Tsikaras PD. Anatomical variations in the branches of the human aortic arch in 633 angiographies: clinical significance and literature review Surg Radiol Anat. 2009; 31(5): 319-23.
- Sokolis DP, Boudoulas H, Karayannacos PE. Segmen- tal differences of aortic function and composition: clinical implications. Hellenic J Cardiol 2008; 49(3): 145-54.
- Demertzis S, Hurni S, Stalder M, Gahl B, Herrmann G, Van den Berg J. Aortic arch morphometry in living humans. J Anat 2010; 217(5): 588-96.
- Jakanani GC, Adair W. Frequency of variations in aortic arch anatomy depicted on multidetector CT. Clin Radiol 2010; 65(6): 481-7.
- Manyama M, Rambau P, Gilyoma J, Mahalu W. A variant branching pattern of the aortic arch: a case report. J Cardiothorac Surg 2011; 13: 6:29.
- Ogeng’o JA, Olabu BO, Gatonga PM, Munguti JK. Branching pattern of aortic arch in a kenyan popula- tion. J. Morphol. Sci., 2010; 27: 51-5.
- Shin IY, Chung YG, Shin WH, Im SB, Hwang SC, Kim BT. A morphometric study on cadaveric aortic arch and its major branches in 25 korean adults : the perspective of endovascular surgery. J Korean Neuro- surg Soc 2008; 44(2): 78-83.
- Layton KF, Kallmes DF, Cloft HJ, Lindell EP, Cox VS. Bovine aortic arch variant in humans: clarification of a common misnomer. AJNR Am J Neuroradiol 2006; 27(7): 1541-2.
- Szpinda M. Morphometric study of the brachiobi- carotid trunk in human fetuses. Ann Anat. 2007; 189(6): 569-74.
- Brauner E, Lapidot M, Kremer R, Best LA, Kluger Y. Aberrant right subclavian artery- suggested mechanism for esophageal foreign body impaction: Case report. World J Emerg Surg 2011; 6(1): 7922-6.
- Alvarez JR, Quiroga SJ, Nazar AB, Comendador MJ, Carro GJ. Aberrant right subclavian artery and calcifiedaneurysm of Kommerell's diverticulum: an alternativeapproach. J Cardiothorac Surg 2008; 3: 8090-3.
- Albayram S, Gailloud P, Wasserman BA. Bilateral arch origin of the vertebral arteries. AJNR Am J Neuroradiol. 2002; 23(3): 455-8.
- Goray VB, Joshi AR, Garg A, Merchant S, Yadav B, Maheshwari P. Aortic arch variation: a unique case with anomalous origin of both vertebral arteries as additional branches of the aortic arch distal to left subclavian artery. AJNR Am J Neuroradiol. 2005; 26(1): 93-5.
- Haifa A, Wafaa S. An anatomical study of the aorticarch variations. JKAU: Med. Sci. 2010; 17: 37-54.
- Best IM, Bumpers HL : Anomalous origins of the right vertebral,subclavian, and common carotid arteries in apatient with a fourvessel aortic arch. Ann Vasc Surg 2002; 16: 231-34.
- Nayak RS, Pai MM, Prabhu LV, D’Costa S, Shetty P. Anatomical organization of aortic arch variations in the India: embryological basis and review. J Vasc Bras 2006; 5: 95–100.