ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 14
A rare localized giant cell tumor of the tendon sheath in the hip joint: A case report and review of the literature
Yong Qin, Bin Zhang and Song-cen LV*
Department of Orthopaedics, Second Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, PR China
- *Corresponding Author:
- Song-cen LV
Department of Orthopaedics
Second Affiliated Hospital of Harbin Medical University
Harbin, PR China
Accepted on June 27, 2017
Giant Cell Tumor of the Tendon Sheath (GCTTS) is the most common benign neoplasm after the ganglion cyst. It is a soft tissue mass that progresses slowly and commonly occurs on the tendon sheath and at the joints of the digits. To date, most case reports have reported GCTTS in the hands. However, GCTTS originating in the hip joint has not been reported to date. Case report: We present a rare case of GCTTS in the hip joint and review the relevant literature. GCTTS of the hip joint is considerably rare. Magnetic resonance imaging is still the first choice of diagnostic modality besides pathological evaluation. Surgery is probably the optimal treatment option to prevent recurrence. In case of bony involvement, reconstructive surgery similar to artificial joint arthroplasty would be an effective treatment option.
Keywords
Giant cell tumor of the tendon sheath (GCTTS), Hip joint, Surgery, Total hip replacement.
Abbreviations
Giant cell tumor of the tendon sheath (GCTTS); Magnetic resonance imaging (MRI).
Introduction
Giant Cell Tumor of the Tendon Sheath (GCTTS) is the second most common tumor affecting the hands after the ganglion cyst. They are mostly benign and develop slowly [1]. The GCTTS has been historically portrayed as pigmented villonodular synovitis, localized nodular tenosynovitis, synovial xanthoma, fibrousxanthoma, xanthomatous giant cell tumor, histiocytic giant cell tumor, benign synovioma, and sclerosing haemangioma, which indicates that the GCTTS is a complicated and multiplicate pathological procedure [2-6]. The etiology of GCTTS is still controversial [7]. While some authors believe that it is a disease of neoplastic nature, others accept it only as a non-neoplastic tumor [8-10]. It can be roughly classified into diffuse type (mostly extra-articular) and localized type (mostly intra-articular) [11,12]. The localized type (tenosynovial giant cell tumor) occurs frequently and represents the most common subset arising from the synovial joint, bursa, or tendon sheath with 85% of the cases occurring in the fingers according to literature, while occurrence at other sites has been relatively less common [5,11,13-15]. Particularly, localized GCTTS growing in the hip joint has not been previously reported. Here, we present a rare case of GCTTS originating at the hip joint, which was treated via surgical excision and total hip joint arthroplasty.
Case Report
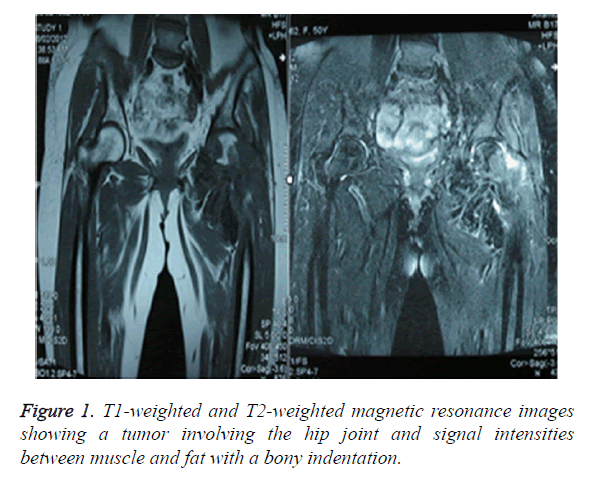
A 50 y old woman working as a farmer, presented with pain in her left hip joint and difficulty in walking for almost one year. Groin tenderness and Faber gestures were detected. Magnetic Resonance Imaging (MRI) showed an abnormal signal around the left hip joint, which produced a significant discrepancy between muscle and fat on T1-weighted and T2-weighted images, accompanied by a bony indentation (Figure 1). Owing to its rarity in the hip joint, GCTTS was not initially identified. The incisional biopsy of the lesions would be the most appropriate course of treatment.
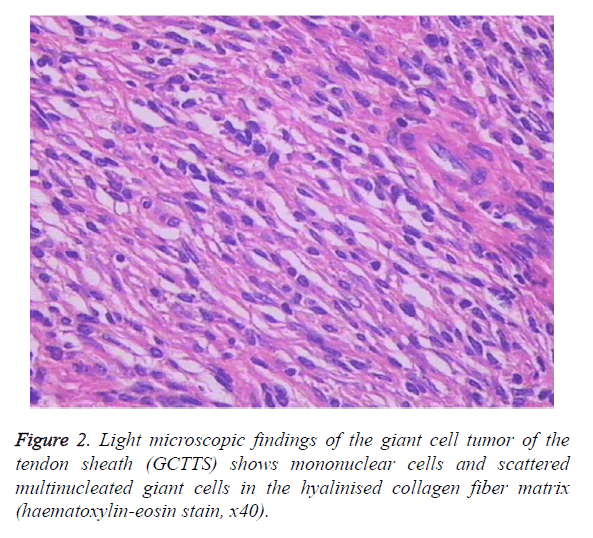
During surgery, a copious amount of yellow soft tissue was found around the hip joint. The masses were nodular with intact capsules. The mean size of the masses was 8 × 10 × 9 mm. The acetabulum and femoral head were invaded and consequently compressed. The analysis of fast-frozen sections showed amounts of mononuclear cells and scattered multinucleated giant cells in the hyalinised collagen fibre matrix, which indicated GCTTS. After meticulous dissection, the tumor, as well as the pathological synovium was completely removed. At this stage, we had not operated on the acetabulum and femoral head. GCTTS was confirmed via postoperative pathological examination (Figure 2).
The patient aggressively developed symptoms of pain and difficulty in walking for two months after the excisional operation, which was consistent with the findings of the first operation. In order to prevent recurrence and metastasis, total hip arthroplasty was performed. Considering the younger age and full activity, we choose the cement less prosthesis of femoral stem and acetabular cup, combined with full ceramic interface. After the second operation, the pain disappeared and the patient regained the ability to walk normally.
Discussion
GCTTS is a proliferative synovial lesion of unknown etiology [6,8,10,16]. Trauma, inflammation, metabolic disease, and neoplastic etiology are considered as etiological factors [17]. Generally, GCTTS can be roughly divided into localized and diffuse types. The localized type, also called nodular tenosynovitis, typically occurs on the digits.
Although GCTTS usually causes no particular symptoms other than a painless, palpable nodule, it induces osseous erosion [18-20]. The radiographic findings of Karasick demonstrated bone erosion in up to 10%-20% of the patients [21].
MRI has a very important role in preoperative diagnosis. The MRI signal intensity of GCTTS was consistent with that of skeletal muscle or that between the muscle and fat on T1- weighted images, while on T2-weighted images, the signal intensity was potentially between that of the muscle and fat [21]. The relatively low signal intensity of GCTTS on T2- weighted images is an important feature that differentiates it from soft-tissue sarcoma, which usually has signal intensity equal to or greater than that of fat on T2-weighted images [22]. Simon et al. reported that preoperative examination with positron emission tomography showed increased activity of surveillance F-18 fluorodeoxy glucose in the lesion [23]. Otherwise, fine needle aspiration biopsy could provide reliable results in the diagnosis of GCTTS [23-25].
Apart from its high incidence in the hands (both flexors and extensors), GCTTS has also been reported in other sites including the toes, deltoid muscle, knee joint, pes anserine bursa, spread forearm, thigh and vertebrae [5,11-15,17,18,26-36]. GCTTS invasion of the parotid gland has also been reported [37]. All these studies show that GCTTS actively and aggressively proliferates, which is inconsistent with previous findings suggesting that GCTTS progresses slowly. However, GCTTS was seldom reported in the hip joint. Gitelis et al. reported a case of pigmented villonodular synovitis (diffuse type GCTTS) in 1989 [38]. However, localized GCTTS with an intact capsule has not been previously reported in the hip joint.
The high recurrence rate of GCTTS is the main challenge in its treatment [1,2,17,19,39]. Surgical incisions should be planned in a way that allows the surgeon to have dorsal and ventral access to tumor extensions. The tumor itself must be dissected gently to avoid potential regional metastasis, which is possible through the resection of the entire tumor with the intact capsule. The cuff of the tendon sheath, part of the capsule, periosteum, or even part of the tendon should be removed if required to ensure the removal of all pathological tissue. To deal with intraosseous invasion, some authors have suggested tumor excision accompanied by the curettage of the involved bone, lavage with 0.25% phenol and cancellous bone graft [40]. In case of extensive bony involvement, the involved bone segment could be totally amputated while preserving the neurovascular bundles, skin, nail and pulp; followed by microsurgical reconstruction [41]. Joint replacement could serve as an alternative for reconstruction following tumor resection, similar to our case. Intra-articular GCTTS can also be resected via arthroscopic treatment. However, the risk of recurrence after the procedure is still uncertain [27].
Unfortunately, recurrence is still a huge challenge concerning the surgical resection of GCTTS. In some cases, the recurrence rate was as high as 50% [27]. The risk factors known to be associated with a high recurrence rate include the proximity to the arthritic joint, proximity to the distal interphalangeal joints of the fingers, proximity to the interphalangeal joint of the thumb and radiological osseous erosions [42]. In a recent study, it was identified that molecular genetics played an important role in the aggressiveness and recurrence of GCTTS [6,16]. Jayant et al. reported that radiation therapy might be helpful in case further surgery is not a good option in recurrent cases [43]. Chemotherapy is also an effective alternative in recurrent cases or where surgery is contraindicated [3].
Consent
Written informed consent was obtained from the patient for publication of her data and any accompanying images. A copy of the written informed consent is available for review by the Editor-in-Chief of this journal.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Acknowledgment
We thank the Department of Pathology at the Second Clinical College of Harbin Medical University, China, for their technical assistance.
References
- Al-Qattan MM. Giant cell tumours of tendon sheath: classification and recurrence rate. J Hand Surg Br 2001; 26: 72-75.
- Martin RN, Osborne DL, Edwards MJ, Wrightson W, McMasters KM. Giant cell tumor of tendon sheath, tenosynovial giant cell tumor, and pigmented villonodular synovitis: defining the presentation, surgical therapy and recurrence. Oncol Rep 2000; 7: 413-419.
- Palmerini E, Staals EL, Maki RG, Pengo S, Cioffi A, Gambarotti M, Picci P, Daolio PA, Parafioriti A, Morris C, Antonescu CR, Gronchi A, Casali PG, Donati DM, Ferrari S, Stacchiotti S. Tenosynovial giant cell tumour/pigmented villonodular synovitis: outcome of 294 patients before the era of kinase inhibitors. Eur J Cancer 2015; 51: 210-217.
- Ravi V, Wang WL, Lewis VO. Treatment of tenosynovial giant cell tumor and pigmented villonodular synovitis. Curr Opin Oncol 2011; 23: 361-366.
- Maheshwari AV, Muro-Cacho CA, Pitcher JJ. Pigmented villonodular bursitis/diffuse giant cell tumor of the pes anserine bursa: a report of two cases and review of literature. Knee 2007; 14: 402-407.
- Nilsson M, Hoglund M, Panagopoulos I, Sciot R, Dal Cin P, Debiec-Rychter M, Mertens F, Mandahl N. Molecular cytogenetic mapping of recurrent chromosomal breakpoints in tenosynovial giant cell tumors. Virchows Arch 2002; 441: 475-480.
- Darwish FM, Haddad WH. Giant cell tumour of tendon sheath: experience with 52 cases. Singapore Med J 2008; 49: 879-882.
- Coster AA. Giant cell tumor of tendon sheath (benign synovioma). J Am Podiatry Assoc 1976; 66: 538-541.
- Kahn LB. Malignant giant cell tumor of the tendon sheath. Ultrastructural study and review of the literature. Arch Pathol 1973; 95: 203-208.
- Vogrincic GS, O'Connell JX, Gilks CB. Giant cell tumor of tendon sheath is a polyclonal cellular proliferation. Hum Pathol 1997; 28: 815-819.
- Sanghvi DA, Purandare NC, Jambhekar NA, Agarwal MG, Agarwal A. Diffuse-type giant cell tumor of the subcutaneous thigh. Skeletal Radiol 2007; 36: 327-330.
- Yoo JH, Yang BK, Park JM. Localized nodular synovitis of the knee presenting as anterior knee pain: a case report. Knee 2007; 14: 398-401.
- Muramatsu K, Mine T, Ichihara K. A typical tenosynovial giant cell tumor of the extensor hallucis longus tendon. J Am Podiatr Med Assoc 2006; 96: 359-361.
- Doita M, Miyamoto H, Nishida K, Nabeshima Y, Yoshiya S, Kurosaka M. Giant-cell tumor of the tendon sheath involving the thoracic spine. J Spinal Disord Tech 2005; 18: 445-448.
- Okutan O, Solaroglu I, Ozen O, Saygili B, Beskonakli E. Tenosynovial giant cell tumor in the cervico-thoracic junction. Turk Neurosurg 2012; 22: 769-771.
- Nishio J, Kamachi Y, Iwasaki H, Naito M. Diffuse-type tenosynovial giant cell tumor with t (1;17) (p13; p13) and trisomy 5. In Vivo 2014; 28: 949-952.
- Hamdi MF, Touati B, Zakhama A. Giant cell tumour of the flexor tendon sheath of the hand: analysis of 27 cases. Musculoskelet Surg 2012; 96: 29-33.
- Chang KJ, Byun BH, Moon HS, Park J, Koh JS, Kim BI, Lim SM. Tenosynovial giant cell tumor of diffuse type mimicking bony metastasis detected on F-18 FDG PET/CT. Nucl Med Mol Imaging 2014; 48: 230-232.
- Pina S, Fernandez M, Maya S, Garcia RA, Noor A, Pawha PS, Som PM. Recurrent temporal bone tenosynovial giant cell tumor with chondroid metaplasia: the use of imaging to assess recurrence. Neuroradiol J 2014; 27: 97-101.
- Enzinger FM, Weiss SH. Benign tumors and tumor like lesions of synovial tissue. Soft Tissue Tumors 1995; 735-755.
- Karasick D, Karasick S. Giant cell tumor of tendon sheath: spectrum of radiologic findings. Skeletal Radiol 1992; 21: 219-224.
- Kitagawa Y, Ito H, Amano Y, Sawaizumi T, Takeuchi T. MR imaging for preoperative diagnosis and assessment of local tumor extent on localized giant cell tumor of tendon sheath. Skeletal Radiol 2003; 32: 633-638.
- Simon SL, Inneh IA, Lee MS, Sullivan S, Ennis F. Tenosynovial giant cell tumor of the thigh: positron emission tomography findings. Am J Orthop 2011; 40: 115-117.
- Abdou AG, Aiad H, Youssef AN. Fine needle aspiration cytology of chondroid tenosynovial giant cell tumor of the hand. Rare Tumors 2015; 7: 5814.
- Wakely PJ, Frable WJ. Fine-needle aspiration biopsy cytology of giant-cell tumor of tendon sheath. Am J Clin Pathol 1994; 102: 87-90.
- Kuhnen C, Muller KM, Rabstein S, Kasprzynski A, Herter P. Tenosynovial giant cell tumor. Pathol 2005; 26: 96-110.
- Aksoy B, Erturer E, Toker S, Seckin F, Sener B. Tenosynovial giant cell tumour of the posterior cruciate ligament and its arthroscopic treatment. Singapore Med J 2009; 50: 204-205.
- Largo RD, Jung FJ, Calcagni M, Jandali AR. Multicentric localised giant cell tumour of the tendon sheath on both hands with a focal infiltration of the extensor tendon: case report and review of the literature. Handchir Mikrochir Plast Chir 2011; 43: 181-185.
- Yun SJ, Hwang SY, Jin W, Lim SJ, Park SY. Intramuscular diffuse-type tenosynovial giant cell tumor of the deltoid muscle in a child. Skeletal Radiol 2014; 43: 1179-1183.
- Lee JH, Wang SI. A tenosynovial giant cell tumor arising from femoral attachment of the anterior cruciate ligament. Clin Orthop Surg 2014; 6: 242-244.
- Kim HS, Kwon JW, Ahn JH, Chang MJ, Cho EY. Localized tenosynovial giant cell tumor in both knee joints. Skeletal Radiol 2010; 39: 923-926.
- Abdullah A, Abdullah S, Haflah NH, Ibrahim S. Giant cell tumor of the tendon sheath in the knee of an 11-year-old girl. J Chin Med Assoc 2010; 73: 47-51.
- Yildiz S, Cetinkol E. Case report: Tenosynovial giant cell tumor arising from the knee joint. Tani Girisim Radyol 2003; 9: 81-83.
- Fnini S, Ouarab M, Cohen D, Trafeh M. Giant cell tenosynovial tumor, spread in the forearm soft tissues. A case report. Chir Main 2001; 20: 236-240.
- Furlong MA, Motamedi K, Laskin WB, Vinh TN, Murphey M, Sweet DE, Fetsch JF. Synovial-type giant cell tumors of the vertebral column: a clinicopathologic study of 15 cases, with a review of the literature and discussion of the differential diagnosis. Hum Pathol 2003; 34: 670-679.
- Dingle SR, Flynn JC, Flynn JJ, Stewart G. Giant-cell tumor of the tendon sheath involving the cervical spine. A case report. J Bone Joint Surg Am 2002; 84: 1664-1667.
- Guo L, Qasem S, Bergman S, Salih ZT. Tenosynovial giant cell tumor presenting as a parotid gland mass: Expanding the differential diagnosis of giant cell-rich lesions in salivary glands. J Cytol 2014; 31: 224-226.
- Gitelis S, Heligman D, Morton T. The treatment of pigmented villonodular synovitis of the hip. A case report and literature review. Clin Orthop Relat Res 1989; 154-160.
- Caputo V, Fiorella S, Orlando E. Postsurgical paracicatricial cutaneous satellitosis of giant cell tumour of the tendon sheath, localized type. Case Rep Dermatol 2011; 3: 118-123.
- Booth KC, Campbell GS, Chase DR. Giant cell tumor of tendon sheath with intraosseous invasion: a case report. J Hand Surg Am 1995; 20: 1000-1002.
- Lu CT, Chen HC, Coskunfirat OK. Immediate toe transfer following index finger amputation for extensive giant cell tumor of the tendon sheath with intraosseous invasion. Chang Gung Med J 2004; 27: 312-317.
- Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheath. J Hand Surg Am 1999; 24: 1298-1302.
- Goda JS, Patil P, Krishnappan C, Elangovan D. Giant cell tumor of the tendon sheath treated by brachytherapy (surface mold) technique-A technical illustration. Brachytherapy 2009; 8: 79-83.